Multipurpose cells could act as biological repair kits, treating diseases that won’t get better on their own
For most of us, minor wounds are just an inconvenience. We endure the minor pain of a cut or scrape, stick on a bandage and within a week, our skin looks like nothing ever happened.
In some cases, though, healing isn’t so simple. Somewhere along the way, the complex chain of events that lets the body repair itself breaks down, and a wound remains open, raw. Such is the case with those who suffer from chronic foot ulcers, a nonhealing wound common in diabetics.
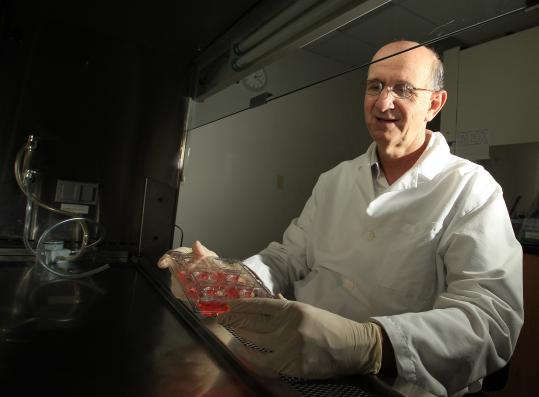
“For these foot ulcers, there are a variety of therapies, but they are only successful in roughly half the cases, and [the ulcers] have a high recurrence rate,” says Jonathan Garlick, head of the Division of Cancer Biology and Tissue Engineering at Tufts School of Dental Medicine. If the wound doesn’t heal, sometimes the only recourse is to amputate the limb.
Garlick’s research could one day help patients avoid that kind of traumatic outcome. He studies pluripotent stem cells—a type of all-purpose cell that has the potential to become any type of tissue in the human body. Once cells like these are harnessed in the lab, he says, researchers can implant them directly into damaged tissue to stimulate healing.
It’s a radical new way of thinking about treating disease, and it offers possible cures for chronic conditions that may not otherwise heal on their own‚ from diabetic foot ulcers to heart disease and even periodontal disease, where lingering inflammation can lead to bone and gum loss.
“There are millions of patients suffering from chronic, nonhealing conditions like these,” says Garlick, a professor of oral and maxillofacial pathology. “That suggests that we have a lot of work to do.”

A microscopic view of fibroblast cells grown from a patient’s nonhealing, diabetic foot ulcer. (Photo: Jonathan Garlick lab)
The challenges he and other pluripotent stem cell researchers face, however, have often been more political than scientific. Until several years ago, the only way to obtain such cells has been to harvest them from human embryos that are several days old; those tiny balls of cells ultimately grow into muscle, nerves, skin and bone in the womb. Because embryos develop from fertilized human eggs, opponents of their use in research argue that scientists should not be allowed to work with them in the lab, a stance that has sparked heated debate over the embryo’s role in the quest for stem cell therapies.
Garlick’s research, however, might allow scientists to sidestep these moral conundrums. Using a process Japanese researchers developed in 2006, he and his team “reboot” cells from freshly removed foreskins (yes, foreskins), forcing them to revert to an embryonic cell-like state by adding four genes to the cells’ DNA. The resulting cells, called induced pluripotent stem (iPS), acquire the ability to develop again into different kinds of cells.
“These alternative cells are really at the crux of our scientific questions,” says Garlick. “Are induced pluripotent stem cells the equivalent to embryonic stem cells in terms of their potential therapeutic value? Do they hold the same promise for human therapies in the future?”
To find out, Garlick and his colleagues are trying to better understand some of the biochemical processes that let the cells “reboot” in the first place. He says it all goes back to DNA—or rather, the myriad ways that cells interpret DNA.
“What’s really special about the epigenome is that it gives cells the ability to regulate which genes are expressed, without altering information stored in the DNA itself”
Genetic Recipes
As you may remember from high school biology, the information in a DNA molecule is a master plan for the entire body. It’s a genetic cookbook of sorts—inside, it contains recipes for creating bone cells, muscle cells, skin cells or any other type of cell. Somehow, though, in the face of all this raw information, cells know exactly where to start reading. A healthy liver cell homes in on recipes relevant to liver cells, and a healthy nerve cell will focus only on recipes that make nerve cells.
This selective reading of DNA is made possible by a biochemical control system called the epigenome. Like a set of bookmarks, it highlights certain sections of DNA, allowing specific genes to “turn on” as a cell develops. The epigenome can also “mask” parts of DNA, effectively turning those genes off. By selecting which genes can be activated at a given time, the system guides cells to develop into specific types.
“What’s really special about the epigenome is that it gives cells the ability to regulate which genes are expressed, without altering information stored in the DNA itself,” says Garlick.
The epigenome is also key to creating iPS cells. The four genes that Garlick’s lab add to skin cells can rearrange these DNA “bookmarks,” making only specific parts of the DNA cookbook (the parts needed to make an embryoniclike cell) available for browsing. As a result, the cell is reprogrammed back to its original embryonic state.
Understanding the epigenome has big implications for understanding disease, Garlick notes. A patient may have flawless DNA, but if his or her cells are reading it wrong, well, there are going to be problems. He thinks these epigenetic glitches might cause some nonhealing disorders—and that iPS cells could offer a tantalizing cure.
“If we can understand the epigenome in iPS, we can think about using cells derived from them to treat a chronic wound or periodontal gum defect that doesn’t heal, and potentially reverse those defects,” he says.
Although iPS cell therapy is promising, it’s not yet a magic bullet. Clinical trials, slated to begin in Japan by March 2014, haven’t yet been approved in the United States. The field is so new, Garlick notes, it’s unclear whether iPS cells can be used in humans without complications. “We have to be 100 percent sure that any cell derived from an iPS won’t give rise to a tumor,” he says. “That’s going to be a big challenge to the field.”

A colony of human-induced pluripotent stem cells. Each of the cells in this cluster has the potential to remain a stem cell or can be stimulated to become a more specialized cell type with therapeutic potential. (Photo: Jonathan Garlick lab)
In the meantime, he and his team are using tissues grown from iPS cells to study diabetic foot ulcers in the lab. “By using iPS-derived cells to engineer skinlike tissues, it’s possible to examine the behavior and biology of diseases in ways we couldn’t do in humans,” he says. “Essentially, we have a surrogate for a human right on our lab bench.”
In a dish filled with orange fluid, he points out a translucent, dime-sized puck. It’s human skin tissue grown from iPS cells. Garlick’s team is using it to examine how the cells might behave once transplanted into a patient. Up close, it looks like an insignificant blurry mass, yet what it represents is something much bigger. By using tissues like these to gain a deeper understanding of what makes new iPS-derived cells tick, Garlick says it may one day be possible to create a sort of biological “repair kit” to treat nonhealing diseases in the mouth and throughout the body.
“Dental research like this contributes to an understanding of basic disease processes that are broadly relevant to the entire body,” he says. “After all, our mission as dentist-scientists is to advance both oral and systemic health—to reduce the burden of disease, and to improve quality of life.”